

Chapter 7: Basic surgical treatment exemplified by thyroid surgery
By Andrew Luzzi and Frank Luzzi, MD
This chapter will illustrate how surgery can be used to treat a pathological condition by detailing the surgical management of a thyroid nodule. The chapter will describe the initial diagnosis, the factors contributing to the decision for surgery, the logistics of the operating room, and the surgical procedure itself.
7.1 Basic thyroid anatomy and functionThe thyroid is an endocrine gland found in the neck. It produces the hormones triiodothyronine and thyroxine, which affect a vast array of metabolic, developmental, and homeostatic processes of the body.
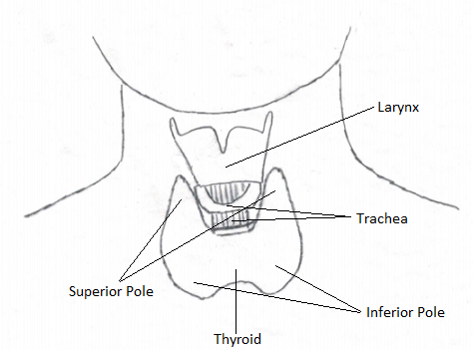
The following is a basic outline of thyroid structure and other related anatomy. The thyroid consists of two lobes with vertically oriented axes that are connected by an isthmus. The top part of a lobe is called the superior pole and the bottom part of a lobe is called the inferior pole. The thyroid is located in the anterior (front) lower neck and is attached to the underlying trachea by two ligaments called Berry's Ligaments. Four small endocrine glands, called parathyroid glands, modulate calcium levels in the body and are physically associated with the thyroid gland but not affiliated metabolically. The superior parathyroid glands are found along the posterior superior surface, and the inferior thyroid glands are adjacent to the inferior poles of the thyroid. Several important blood vessels and nerves are also in close proximity to the thyroid.
7.2 Diagnosis of a thyroid nodule
A thyroid nodule may initially be suspected when a patient feels a lump in their lower neck, a physician feels the lump during a routine physical exam, or a physician finds the nodule on a radiologic exam for an unrelated problem. In any case, the physician will palpate the thyroid with the patient swallowing and not swallowing. Swallowing shifts the gland superiorly, at times allowing a better evaluation of the nodule. If the physician determines that there is a problem, an ultrasound of the gland will be performed to confirm the nodule's presence. If the nodule appears on this exam to have concerning features, such as calcifications, a certain minimal size, usually 5mm, or a complex nature (part solid and part cystic), a fine needle aspiration biopsy will be ordered. This biopsy of the nodule will be sent for cytologic evaluation. The cytology results will dictate the treatment taken. If the nodule is felt to be benign, the thyroid may continue to be monitored or no further evaluation may be required. If the cytology shows concerning features, such as atypia of the genetic material, monitoring or surgical intervention will be decided upon. If there is a strong suspicion for cancer, surgery will be recommended.
This chapter will assume that the patient has a 1.5cm nodule in the right thyroid lobe having concerning features but not outright malignant changes on cytology. The physician will then discuss the option of a right hemi thyroidectomy with the patient and its associated risks and benefits. The physician will explain to the patient that the right side of the thyroid, once removed, will be sent to the pathology department while the patient is still on the operating room table to determine if the nodule is cancerous. The pathologist will determine whether or not the nodule is a cancer and will relay this information back to the operating room and surgeon. If the nodule is cancerous, the surgeon may then remove the remaining thyroid gland.
7.3 Pre-surgical treatment and planning
Before the patient undergoes surgery, he must have several tests. The physician will ensure that the vocal cords are performing normally by mirror or fiber optic exam. Vocal cord function can be compromised by the cancer itself or by trauma during the surgery. Additionally, prior to the surgery, laboratory tests will determine the baseline level of thyroid and parathyroid function. Specifically, thyroid stimulating hormone level, which correlates to thyroid function, and ionized calcium level, which correlates to parathyroid function, will be measured. Thyroid function is often reduced proportionately to the amount of thyroid surgically removed. Parathyroid function may be impaired, as the glands are so small and intimately associated with the thyroid that they may be directly damaged, their vasculature may be compromised, or at times they may be removed inadvertently during surgery.
Also prior to the surgery, the physician will outline the risks of the operation to the patient. These include risks of bleeding, infection, and scar formation, risk of damage to the nerves that supply the voicebox, and risk of damage to the parathyroid glands.
The patient is brought into the operating room and general anesthesia induced. The patient is intubated with an endotracheal tube that has electrodes that connect to a nerve integrity monitor and are positioned at the level of the vocal cords. If the nerve that innervates the muscles to the vocal cords, the recurrent laryngeal nerve, is manipulated during surgery, the vocal cord will move and the electrodes will send a signal to the nerve integrity monitor which will alert the surgeon with an audible beep. The importance of this device will be highlighted later in the chapter.
The surgeon scrubs his hands with antibacterial soap outside of the operating room. Upon entering the operating room, the surgeon dons a gown, gloves, and a headlight with assistance from the nurses. The patient is positioned in a neck extended position. This means that the chin is up and the head is back. This position is achieved with the help of a roll positioned beneath the shoulders of the patient. This position elongates the neck and makes the thyroid easier to access. After cleaning the neck with alcohol, the surgeon palpates the thyroid notch and approximately two finger breadths superiorly draws a gently curved line with a marker in a natural skin crease extending from one sternocleidomastoid muscle to the other. This demarcation is then injected with 1% lidocaine with a dilution of 1:100,000 epinephrine to provide a local anesthetic and vasoconstrictive effect. The patient is prepped with betadine extending from the chin to the superior aspect of the chest and as far lateral right and left as possible. Then, sterile drapes are placed to isolate the field of interest - the anterior neck.
As the nodule is in the right thyroid lobe, the surgeon approaches the operating table and stands on the patient's right. Across from the surgeon is his assistant. To the surgeon's right stands the scrub nurse, who will hand equipment to the surgeon throughout the case.
7.5 The operation, part I: obtaining exposure to the surgical field
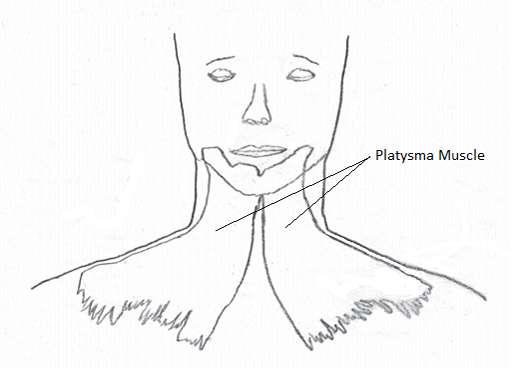
The surgeon makes an incision along the line of demarcation, cutting sequentially through skin, subcutaneous tissue, and the platysma muscle (a superficial muscle covering most of the neck) with a sharp, steel knife. The platysma muscle is invested in fascia - a fibrous connective tissue. Beneath this fascia, the surgeon uses electrocautery or sharp scissors to separate this flap of skin, subcutaneous tissue, muscle, and fascia from the underlying structures of the neck, both superiorly and inferiorly. These flaps are then retracted using retaining sutures. The surgeon has now gained exposure to what will be the surgical field.
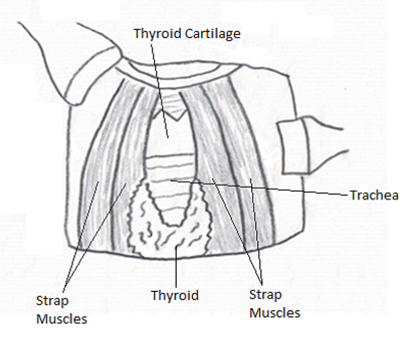
What the surgeon initially sees are strap muscles - a group of four pairs of muscle in the anterior part of the neck covering the trachea, cricoid cartilage, and larynx. The linea alba refers to a line that separates the left and right strap muscles. The surgeon begins the second part of the operation by grasping the midline of the strap muscles just below the cricoid cartilage in an attempt to locate the linea alba. Then sharply, the linea alba is incised, separating the strap muscles right and left. The surgeon then bluntly retracts the strap muscles and separates them from the underlying thyroid gland. For this particular case, this is primarily done on the right side, leaving the left thyroid lobe only partially visible.
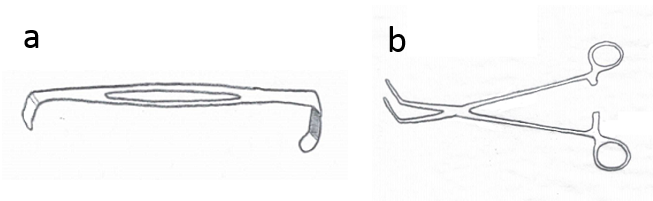
Attention is then directed at the superior thyroid pole. An Army-Navy retractor is placed under the superior flap, and strong retraction is often required to expose the pole. The surgeon will gently dissect overlying tissues away from the superior pole of the thyroid using a clamp with a spreading action or a fine piece of cotton held in a clamp in a pushing fashion. He will then, with the same instruments, isolate the superior thyroid artery and vein. Once done, these vessels are separately clamped, incised, and ligated, often using right angled clamps. The surgeon is careful not to extend his dissection beyond the superior extent of the thyroid, so as not to damage the nearby superior laryngeal nerve, which innervates the cricothyroid muscle that tenses the vocal cords.
Next, attention is directed at the lateral aspect of the thyroid lobe, where blunt dissection is utilized to isolate the middle thyroid vein. Once done, this vein is double clamped, incised, and ligated as close to the capsule of the gland as possible. During this dissection, the surgeon is cognizant of the possible existence of the non-recurrent, recurrent laryngeal nerve.
Throughout the thyroid surgery, and very often during this lateral dissection, many small blood vessels are encountered, which may be tied with suture ligature, cauterized with bipolar cautery, or cut with a harmonic scalpel.
The surgeon now directs his attention to the inferior pole. The surgeon isolates the inferior thyroid artery, but does not yet ligate it due to its close proximity to the recurrent laryngeal nerve. The recurrent laryngeal nerve supplies all of the intrinsic muscles of the larynx, except for the cricothyroid muscles, and is in contact with the posterior medial aspect of the thyroid gland, placing it at significant risk during thyroid surgery. Until the recurrent laryngeal nerve is located, blunt dissection only is used during inferior pole dissection. Most often, this nerve is located in a triangle between the trachea, the inferior pole of the thyroid, and the carotid artery. The surgeon performs blunt dissection with a Crile clamp and a Peanut Dissector. Locating the recurrent laryngeal nerve, which appears to be a white strand, he confirms the nerve's presence by touching it with an electrode which triggers a response in the nerve integrity monitor.
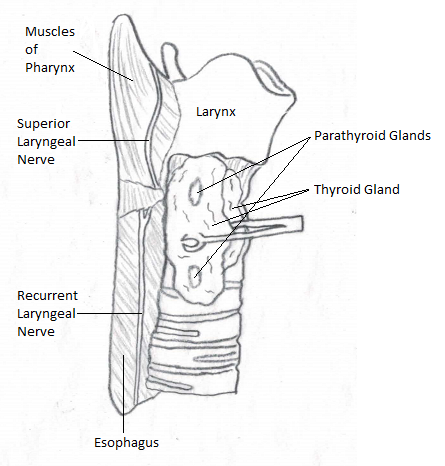
With the nerve located, the surgeon directs his attention to the inferior thyroid artery and the nearby inferior parathyroid gland. The inferior thyroid artery is then double clamped along the inferior pole of the thyroid gland, incised, and ligated. The inferior parathyroid gland is then bluntly dissected away from the inferior pole, out of harm's way. Next, the thyroid isthmus is elevated off of the trachea with a Kelly clamp. The isthmus is then clamped in its entire length on both the right and left side with Kelly clamps and then incised and ligated.

Attention is then redirected at the previously located recurrent laryngeal nerve inferiorly. Placing gentle inferior traction on the nerve using a moistened gauze pad, the surgeon dissects tissues off of the nerve using a Crile clamp in a superior direction. These tissues, including Berry's ligament, are then incised sharply, further exposing the nerve and releasing the thyroid lobe from its tracheal attachment. This process is continued until the nerve is seen to enter the larynx superiorly. Bleeders are often controlled during this step using a bipolar cautery.
The superior parathyroid gland is then found along the superior posterior surface of the thyroid. This gland, in addition to the remaining tissues binding the thyroid deeply, is sharply dissected and the right thyroid lobe is removed from the patient and sent to pathology.
7.8 The operation, part IV: conclusion
During the 15-20 minutes it takes for the pathologist to examine the nodule in question, the surgical bed is irrigated with sterile water and any bleeding vessels are localized and cauterized or tied off with sutures.
If pathology shows that the nodule is benign, which this chapter will assume it does, a drain is placed in the surgical bed, the wound is closed, and a dressing is applied. A drain is a tube used to prevent the accumulation of blood in the wound bed. The drain placed may be a closed system, which uses a vacuum bulb, or an open system, which acts as a wick and allows blood to seep into an overlying dressing.
If the pathology shows that the thyroid nodule is cancerous, the surgeon will often remove the remaining left thyroid lobe.
The wound is closed in layers. The platysma is re-approximated using absorbable sutures, followed by the subcutaneous tissues and then the skin. Most often, the skin is closed with a subcuticular non-absorbable stitch, which is removed 10 days post operatively. Certain glues have also been used for closure of the skin. A moderate pressure dressing is then applied with layers of thick gauze.
The patient is awakened and extubated after the operation and their vocal cords are examined. They are kept in the hospital overnight and so long as there has been only modest blood loss through the drain, the drain is then removed. The patient's ionized calcium level is checked to assure that there is acceptable parathyroid gland function. Thyroid hormone levels are checked in four weeks, as they take this long to show any significant change. If the thyroid function is low, thyroid hormone therapy is prescribed.