

Chapter 6: Basic medical devices - surgical tools
By Andrew Luzzi
During the Clinical Summer Immersion program at Cornell University, the Biomedical Engineering students witnessed numerous operations and observed the variety of instruments and devices used in surgical procedures. The completion of one surgery typically involves many steps and different techniques, and, as such, a multitude of surgical equipment exists to aid the surgeon in whatever task is required. A myriad of surgical tools are currently used in modern medicine, but many can be organized based on function. This chapter will examine the basics of surgical equipment.
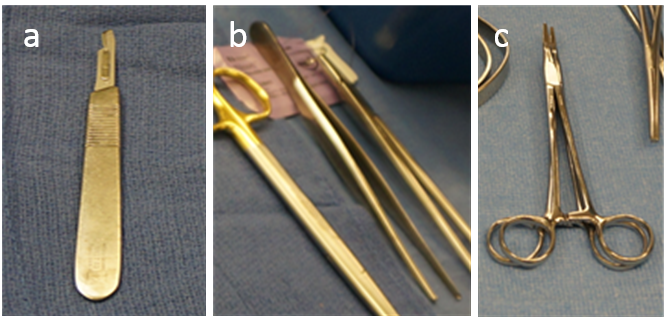
6.1 Tools to cut tissue and exposure the bodyMany surgical tools are simple instruments that allow the surgeon to mechanically manipulate tissue. The scalpel, a staple of the surgeon's arsenal, comes in various shapes and sizes but always consists of a handle and a blade. It is commonly used for initial incisions, as well as cutting through deeper skin layers, muscle, and fat. Surgical scissors, like scalpels, are also used for cutting through skin, muscle, and fat. They resemble standard scissors, but are often smaller so they may be manipulated in limited space and sharper so they may cut through tissue with less resistance.
In order to grasp and manipulate tissue so that it may be dissected, forceps are used. The term forceps can refer to instruments that look like what are commonly referred to as "tweezers" or may refer to instruments that superficially resemble scissors, but instead of sharp blades forceps have a variety of non-cutting appendages to use for various purposes. Duval's forceps, for example, have wide and dull extensions to minimize trauma when grasping delicate tissue such as stomach or lung.
Clamps are a subset of surgical forceps which have a handle mechanism that allows surgeons to lock the appendages closed. These are frequently used to clamp blood vessels during operations. Retractors, on the other hand, are used by surgeons to separate the edges of an incision. Some retractors are simple and consist of a hooked blade with a handle, others are similar to scissors and possess two dull curved blades that can be spread apart, and others are more complicated still. Regardless of their appearance, retractors are used to spread more superficial tissue apart so that the underlying tissue can be viewed. These tools are the basic surgical instruments used to cut, clamp, separate, and maneuver different tissue throughout an operation.
6.2 High-tech tools for tissue manipulation
In addition to these instruments, there are many more technologically advanced devices being used to manipulate and expose tissue as well. One device, termed a laser scalpel, uses laser light to cut through tissue. The light is typically produced by running an electric current through a specific type of gas and the frequency of the light produced varies depending on the gas used. Different frequencies of light, produced using different gases, have distinct functions in surgery. A CO2 laser produces infrared light and is used to ablate soft tissue with high water content, such as fat (http://www.intechopen.com/books/co2-laser-optimisation-and-application). An excimer laser, which uses a dimeric or heterodimeric molecule that decays and releases electromagnetic radiation, produces light in the ultra violet range and is used for eye surgeries. Using lasers can be advantageous for several reasons. Notably, lasers cauterize blood vessels as they cut and thus minimize the amount of bleeding that occurs during an operation. Additionally, lasers make very precise cuts and therefore minimize unnecessary damage to healthy tissue.
Though not as delicate as lasers, drills also have several surgical applications. Drills are used primarily to penetrate hard, dense tissue such as bone. Many neurosurgical procedures require the use of a drill to penetrate the skull and expose the underlying brain and many orthopedic procedures require drills to facilitate the implantation of screws into bone.
Arthroscopic shavers are another motorized tool that serve multiple functions in surgery. A shaver consists of a long, hollow steel rod with a rotating blade at one end. When the surgeon squeezes the rotating hand piece attached to the arthroscopic shaver, the blade rotates. The rotating blade not only sheers and cuts tissue, but also, due to the suction created by the rotation, sucks detached tissue into the blade and away from the area of operation. The arthroscopic shaver is ideal for shaving loose tissue and clearing debris from surgical sites.
While scalpels, drills, and lasers can expose the body for surgery, in order to close wounds resulting from surgery, trauma, or pathology, other devices must be used. The most basic sealing device is the suture. Surgical sutures, consisting of a needle and a thread and colloquially referred to as stiches, differ from the common stich in several ways. Surgical sutures are made from a variety of natural sources, such as collagen and stainless steel, and synthetic sources, such as Nylon and Polysorb, and have a number of variable characteristics. The ideal suture has flexibility, high tensile strength, and the ability to hold when knotted. Additionally, ideal sutures are resistant to infection and cause minimal tissue reaction. Composed of several filaments, a multifilament suture is more flexible and has higher tensile strength than a monofilament suture. However, monofilament sutures, which retain less water than multifilament sutures, typically elicit a lower tissue reaction.
Additionally, all sutures can be classified as either absorbable or non-absorbable. Absorbable sutures degrade in the body over time and can be beneficial to close internal wounds, eliminating the need to re-open the patient, or close superficial wounds, eliminating the need to take out the sutures. Non-absorbable sutures do not degrade in the body and are typically used to close wounds that have a lengthy healing period. Additionally, modern sutures are hypoallergenic, thus preventing allergic reactions to the suture, and many are also coated with antimicrobial substances to mitigate infection.
Tissue adhesives, made from cyanoacrylates - the same compound from which super glues are derived, can be used to repair small and superficial wounds and lacerations. Modern tissue adhesives are able to be stored and applied in liquid form. Upon contact with the skin (or other water containing substances), the adhesive polymerizes, creating an anti-microbial seal over the wound. Using tissue adhesives to close wounds eliminates the discomfort associated with the input of sutures. The use of tissue adhesives also eliminates the suture removal process and typically saves time.

Vacuum-Assisted Closure, pioneered by plastic surgeons at Wake Forest, is a recent technological advance in the treatment of wounds. While able to treat acute wounds, this method is more typically used for chronic wounds and burns. In vacuum-assisted closure, also referred to as negative pressure wound therapy, a piece of foam is initially fitted and placed into the wound and an adhesive membrane is then placed on top of the foam. A drainage tube is fitted through an opening in the film in order to collect fluids. Fitted through another hole in the film, a vacuum pump creates a partial vacuum in the wound by applying negative pressure to the location. The adhesive membrane prevents the inflow of air, which would disrupt the vacuum, and the foam helps to expose every part of the wound to a uniform negative pressure. The vacuum is believed to "[assist] with the removal of interstitial fluid, decreasing localized oedema and increasing blood flow." http://www.worldwidewounds.com/2001/may/Thomas/Vacuum-Assisted-Closure.html
Replacement skin and skin like substances can also be used to repair skin trauma. Autologous skin grafts, where the skin is grafted from a different place on the same individual, and allogenic skin grafts, where the skin is grafted from another person, typically a cadaver, have been used extensively to treat skin trauma, but have several disadvantages. Autologous skin grafts may be disadvantageous because of the limiting amount of skin able to be grafted from the patient, and allogenic skin grafts may result in rejection by the patient or rejection. To improve treatment of skin trauma, synthetic skin has been developed. The type of synthetic skin can vary, but most is composed of a collagen scaffold that is often seeded with the patient's own cells. Applied so that it covers the wound, artificial skin promotes the growth of new skin cells and protects the patient from dehydration and infection. Many aspects of artificial skin and its application are currently being investigated and tested, and it is possible that spray on skin, skin created from spider silk scaffolds, and skin that uses semiconductors to sense touch will be used in the clinic in the future.
http://news.discovery.com/tech/artificial-skin-spider-silk-110810.htm
While sutures and adhesives close superficial wounds, bone cement is used to close gaps inside the body related to artificial joints. When a prosthesis is surgically inserted and attached to a bone, a free space exists between the bone and prosthesis. This free space is filled with bone cement, which serves the functions of both anchoring the prosthesis to the bone and increasing the absorptive ability of the artificial joint. Bone cement initially consists of two phases, one powder, frequently PMMA based, and one liquid, frequently an MMA monomer, which are mixed together. One of the phases typically contains an initiator, and upon mixing, free radical polymerization occurs and the viscosity of the cement steadily increases. The cement is applied as a viscous, doughy, liquid and eventually hardens into a solid.
http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0104-66322011000200007
6.4 Minimally invasive transluminal devices
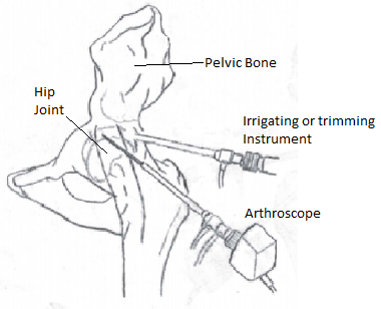
A relatively recent advancement in surgery, endoscopic techniques have spawned many minimally invasive surgical procedures along with various new pieces of surgical equipment. Endoscopic surgery refers to surgical procedures in which a scope is inserted through a natural body opening or a small incision. Minimally invasive procedures have several advantages, including in many cases a decreased risk of infection, a faster recovery, and a smaller scar. The staple of endoscopic procedures is the endoscope. The endoscope has a flexible shaft that, on one end, has a camera and a light. This part of the endoscope is inserted into the body and allows the physician to view the desired internal area of the patient. The images of objects are typically relayed to the eyepiece on the handle of the endoscope using fiber optics or are projected onto a screen using a camera. In addition to frequently containing an eyepiece, the handle of the endoscope also has controls that allow the physician to manipulate the part of the scope that is being inserted into the patient. In order to perform additional medical functions, the endoscope has a channel through which other medical instruments can be inserted. It is through the joint functions of visualization and a combination of cutting, shaving, and manipulating tissue that the endoscope enables a physician to repair torn joint tissue, remove impaired gall bladders, perform bypass surgery, and treat various other medical conditions in a minimally invasive fashion.
In addition to endoscopic techniques, robotic surgery has recently become more popular and has revolutionized the way various operations are performed. Robotics are used to operate in order to reduce the amount of human error involved in surgery. Through several methods, robotic surgery provides the benefit of clean, quantified surgical movements, the preciseness of which cannot be obtained using exclusively a human hand. The exactness of robotic surgery allows for smaller incisions, more efficient cuts, and the option to perform some surgeries using minimally invasive technique that previously required open technique. These advantages of robotic surgery can lead to less blood loss, less tissue damage, smaller scars, and a shorter recovery time. One method of robotic surgery uses a telemanipulator, which involves a pair of robotic arms performing the surgery and a surgeon controlling the arms by carrying out typical surgical movements. Another method, appropriately deemed computer-controlled surgery, involves a surgeon using a computer to control the actions of the robotic arms. Valve repairs, pancreatectomies, hysterectomies, joint replacements, and many other surgeries in various surgical specialties have been performed with the assistance of robotics. Despite some clear advantages of robotic surgery, it also tends to cost more and the long term health benefits of robotic vs. non robotic surgery are not conclusive. Regardless, robotic surgery remains a viable method of performing many surgeries today and there is no doubt that with increasing technological advancement the scope and effectiveness of robotic surgery will continue to increase in the future.
During many surgical procedures, fluids are introduced and/or removed from operation sites. An irrigator is used to flush a wound or operation site with fluid. The passing of fluid over an operation or wound site clears away debris, which both improves visibility and discards material that could be disruptive to the surgeon or pathogenic in nature. The irrigation fluid may also be used to achieve wound hydration. When irrigating a wound, the irrigation equipment, the method of irrigation, the composition of irrigation solution, and the pressure at which the irrigation solution is kept are all taken into consideration. Bulb syringes and piston syringes are two cost effective pieces of equipment that can facilitate wound irrigation. However, the low pressure provided by these syringes may not be as effective at clearing debris and decreasing bacterial load. More elaborate devices that provide pulsed, high pressure irrigation are frequently high cost and cumbersome. Pressurized canisters are also viable pieces of equipment to facilitate the irrigation of wounds. These canisters are relatively inexpensive and can provide high pressure irrigation, however the canister reliability and the warming of the solution in the canister to room temperature can be problematic.
Irrigation solution, in addition to other fluids such as blood, saliva, and other bodily secretions, must frequently be removed from the patient's body during surgery in order improve visibility and clear debris and pathogens. Many hospitals have central vacuum systems, which involve the creation of a vacuum by a device somewhere in the hospital. Many tubes are connected to this device and are directed to other rooms in the hospital, such as operating rooms. In the operating room, a surgeon is able to connect a variety of instruments to the tubing of the central vacuum system. The specific instrument to be used depends on the specific task that must be accomplished. A surgeon may use a thin, smaller instrument called a Frazier suction tip when dealing with small surgical settings. A larger instrument, called a Yankauer suction tip, may be used for larger surgical settings.

A vast array of surgical equipment exists to assist surgeons in the execution of the many different surgical procedures. This chapter covers some basic categories of surgical equipment, but many medical tools and devices not mentioned in this chapter exist and have important clinical uses. With perpetual technological and medical advancement arises the unremitting demand for improved and novel medical devices, notably surgical equipment. Biomedical engineers, being at the forefront of the development of novel medical technology, must have a solid grasp of the current and potential future environment of surgical equipment in order to be best prepared to make significant technological advancements.